Abstract
Background: Acute lymphoblastic leukemia (ALL) is a malignant lymphoproliferative disease. Although the prognosis of ALL patients has improved significantly in recent years, the 5-year overall survival (OS) rate of adolescent and adult patients is still less than 40%. Recurrence after remission of standard chemotherapy is the most important condition affecting survival, response to initial treatment is the key factor to predict the risk of recurrence, and post-remission therapy (PRT) is an important means to prevent recurrence. In addition, there is growing evidence that minimal residual disease (MRD) plays an important role in the treatment and prognosis assessment of ALL patients, and it is necessary to further stratify the risk of ALL patients to determine who will benefit from chemotherapy or HSCT, and to determine the significance of MRD levels in HSCT decisions in ALL patients. Therefore, we conducted a multicenter study based on MRD levels in adolescent and adult ALL patients to explore the clinical and prognostic significance of post-chemotherapy MRD levels in PRT selection in adolescent and adult ALL patients.
Methods: The basic characteristics, cytogenetics, molecular genetics, MRD level, treatment regimen and survival outcome of 404 patients with ALL diagnosed for the first time in Shandong Provincial Hospital, Yantai Yuhuangding Hospital and the Affiliated Hospital of Qingdao University from January 1, 2014 to December 20, 2021 were collected, and the correlation and survival analysis were carried out by SPSS25 software.
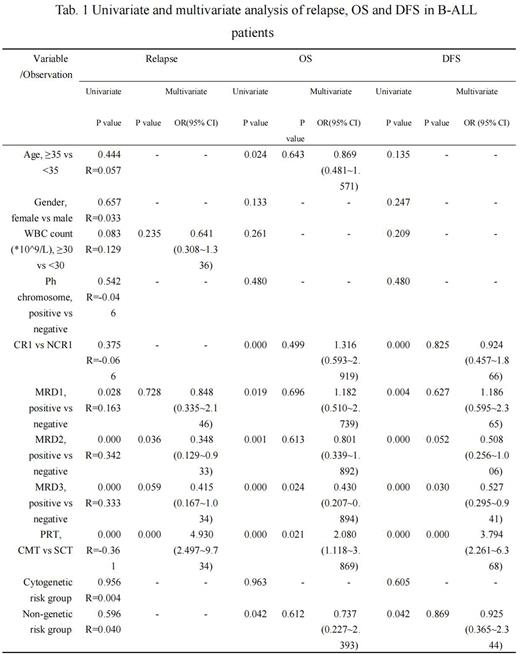
Results: We studied the effect of MRD levels on the prognosis of patients with B-ALL after chemotherapy, and the guiding significance of different MRD after one course of chemotherapy (MRD1) levels for PRT selection. A total of 182 B-ALL patients with MRD data were included in this part, and the prognosis of patients was analyzed. The results of univariate analysis showed that complete remission was achieved after one induction chemotherapy, MRD1 < 0.01%, MRD after two courses of chemotherapy (MRD2) < 0.01%, MRD after three courses of chemotherapy (MRD3) < 0.01%, patient with standard risk of non-genetic risk stratification and patients in stem cell transplantation (SCT) group had better OS and disease-free survival (DFS), while those older than 35 years old had worse OS (P=0.024). In the multivariate analysis, only MRD3 <0.01% and the way of PRT (CMT or HSCT) were independent prognostic factors for OS and DFS. What's more, MRD2 ≥0.01% (P=0.036) and patients grouped into the chemotherapy (CMT) group (P=0.000) was significantly associated with a high risk of recurrence. Patients were divided into four groups according to the time they reached negative MRD, subgroup A (MRD1−/MRD2±/MRD3±); subgroup B (MRD1+/MRD2−/MRD3±); subgroup C (MRD1+/MRD2+/MRD3−); subgroup D (MRD1+/MRD2+/MRD3+); The results showed that the 5-year OS of subgroup A, B, C and D were 64.75%, 52.15%, 43.85% and 24.32% (P=0.000), and the 5-year DFS were 50.17%, 57.27%, 17.38% and 7.35% (P=0.000), respectively. Achieving negative MRD before transplantation was significantly associated with better OS and DFS.
In addition, among the patients with negative MRD1, there was no significant difference in OS between the SCT group and the CMT group. The 5-year OS was 71.9% and 60.9% (P=0.176), respectively. The 5-year DFS was 68.6% and 27.1%, respectively (P=0.004). The recurrence rate in the CMT group was significantly higher than that in the SCT group (45.95% vs 21.43%, P=0.041), but the response rate (64.71%) and survival rate (52.94%) to retreatment after recurrence were high. The prognosis of patients with positive MRD1 was poor. The 5-year OS of patients in CMT group and SCT group were 23.0% and 62.6% (P=0.000), respectively.
Conclusion: The earlier the patients were MRD negative after chemotherapy, the better prognosis would achieve. For the patients achieve negative MRD early after chemotherapy, although there was no significant difference in OS between the chemotherapy group and the transplantation group, allo-HSCT could significantly reduce the recurrence rate and obtain better DFS. Of course, this needs to be further verified in prospective randomized controlled trials.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal